Menopause and Bone Density Loss: A Comprehensive Guide
Imagine your bones as a bustling city, constantly under construction. Old bone tissue is broken down (resorption), and new bone tissue is built (formation). During youth, the construction crew is working overtime, ensuring a sturdy and resilient infrastructure. But as we age, especially during menopause, the construction pace slows, and the demolition crew gains momentum, leading to potential cracks and weakening of the city's foundations. This imbalance is a simplified explanation of what happens to bone density during menopause, making women particularly vulnerable to osteoporosis and fractures.
Understanding Bone Density and Why It Matters
Bone density, or bone mineral density (BMD), measures the amount of calcium and minerals packed into a specific volume of bone. Think of it as the concrete strength of your skeletal system. The higher the density, the stronger and more resistant your bones are to fractures.
Why is Bone Density Important?
Bone density is a critical indicator of bone health. Low bone density signifies that bones are porous and fragile, increasing the risk of breaks from minor falls or even everyday activities like bending over or coughing.
- Strong Bones, Active Life: Healthy bone density ensures an active and independent lifestyle as we age, allowing us to participate in activities we enjoy without fear of fractures.
- Prevents Osteoporosis: Maintaining adequate bone density is crucial in preventing osteoporosis, a condition characterized by weakened bones and increased fracture risk.
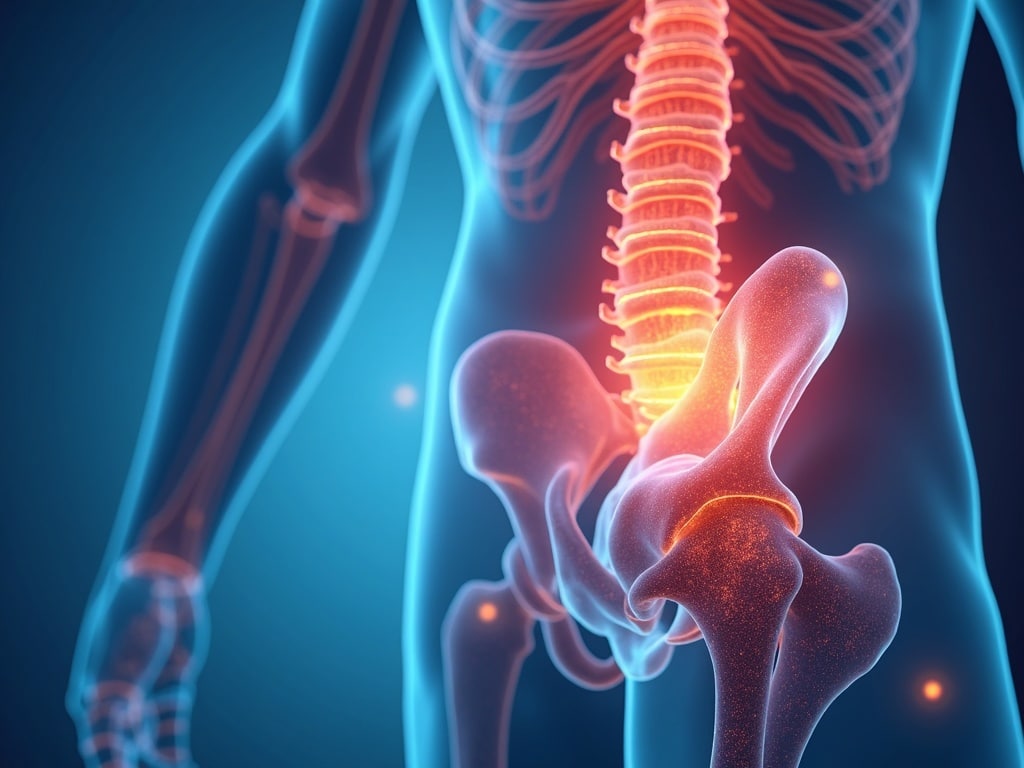
- Reduces Fracture Risk: Higher bone density directly translates to a lower risk of fractures, especially in the hip, spine, and wrist – common sites for osteoporotic fractures.
The Link Between Menopause and Bone Density Loss
Menopause, marking the end of a woman's reproductive years, brings about significant hormonal changes, most notably a decline in estrogen levels. Estrogen plays a vital role in maintaining bone density, acting like a foreman on that construction site, ensuring bone formation keeps pace with bone resorption.
Estrogen's Role in Bone Health
Estrogen influences bone health in several ways:
- Promotes Bone Formation: It stimulates osteoblasts, the cells responsible for building new bone tissue.
- Inhibits Bone Resorption: Estrogen slows down the activity of osteoclasts, the cells that break down old bone.
- Enhances Calcium Absorption: It aids in calcium absorption from the gut, providing the essential building block for bone.
How Menopause Accelerates Bone Loss
When estrogen levels plummet during menopause, the balance between bone formation and resorption is disrupted. Bone resorption outpaces bone formation, leading to a rapid decline in bone density, particularly in the first few years after menopause. This accelerated bone loss is why women are at a significantly higher risk of developing osteoporosis than men.
Risk Factors for Bone Density Loss During Menopause
While all women experience a decline in estrogen during menopause, certain factors can increase the risk of significant bone density loss:
- Early Menopause: Experiencing menopause before the age of 45 increases the duration of estrogen deficiency and the risk of osteoporosis.
- Family History: A family history of osteoporosis or fractures suggests a genetic predisposition to lower bone density.
- Low Body Weight: Women with a low body mass index (BMI) have less bone mass to begin with, making them more vulnerable to bone loss.
- Lifestyle Factors: Unhealthy habits like smoking, excessive alcohol consumption, and a sedentary lifestyle contribute to bone density loss.
- Calcium and Vitamin D Deficiency: Inadequate intake of these essential nutrients impairs bone health.
- Certain Medical Conditions and Medications: Conditions like hyperthyroidism, celiac disease, and long-term use of corticosteroids can negatively impact bone density.
Diagnosing Bone Density Loss: The DEXA Scan
The gold standard for measuring bone density is a dual-energy X-ray absorptiometry (DEXA) scan. This non-invasive test uses low-dose X-rays to measure the mineral content of bones, typically in the hip and spine.
Understanding Your DEXA Scan Results
DEXA scan results are reported as T-scores, which compare your bone density to that of a healthy young adult of the same sex.
- T-score of -1.0 or higher: Normal bone density.
- T-score between -1.0 and -2.5: Osteopenia, indicating lower than normal bone density and an increased risk of osteoporosis.
- T-score of -2.5 or lower: Osteoporosis, indicating significantly weakened bones and a high risk of fractures.
Regular DEXA scans are recommended for women after menopause, especially those with risk factors for osteoporosis. Discussing your risk factors and DEXA scan results with your doctor is crucial for developing an appropriate management plan.
Strategies to Prevent and Manage Bone Density Loss During Menopause
While bone loss during menopause is a natural process, proactive steps can be taken to minimize its impact and maintain strong bones.
Lifestyle Modifications
- Calcium-Rich Diet: Aim for 1200 mg of calcium daily from sources like dairy products, leafy green vegetables, fortified foods, and calcium supplements.
- Vitamin D Supplementation: Vitamin D is essential for calcium absorption. Most adults need 600-800 IU of vitamin D daily, but your doctor may recommend a higher dose based on your individual needs.
- Weight-Bearing Exercise: Engage in activities that force your body to work against gravity, such as walking, jogging, dancing, and weightlifting. These exercises stimulate bone formation.
- Quit Smoking: Smoking significantly impairs bone health.
- Limit Alcohol Consumption: Excessive alcohol intake can interfere with calcium absorption and bone formation.
Medical Treatments
Several medications are available to prevent and treat osteoporosis. Your doctor can help you determine if medication is right for you based on your individual risk factors and bone density.
- Bisphosphonates: These medications slow down bone resorption and are commonly prescribed for osteoporosis.
- Selective Estrogen Receptor Modulators (SERMs): SERMs mimic the beneficial effects of estrogen on bone without the risks associated with hormone therapy.
- Hormone Therapy (HT): HT can effectively prevent bone loss, but it's typically reserved for women with significant menopausal symptoms due to potential risks.
- Calcitonin: This hormone inhibits bone resorption and can be administered as a nasal spray or injection.
- Denosumab: This injectable medication blocks a protein that promotes bone resorption.
- Anabolic Agents: These medications, such as teriparatide and abaloparatide, stimulate bone formation and are typically reserved for individuals with severe osteoporosis.
The Importance of Early Intervention
The key to managing bone density loss during menopause is early intervention. Talking to your doctor about your risk factors, getting regular DEXA scans, and adopting a healthy lifestyle can significantly reduce your risk of osteoporosis and fractures. Don't wait until you experience a fracture to address your bone health.
Living Well with Healthy Bones After Menopause
Menopause is a natural transition, and while it brings about changes in bone health, it doesn't have to define your quality of life. By understanding the connection between menopause and bone density loss, taking proactive steps to protect your bones, and working closely with your healthcare provider, you can maintain strong, healthy bones and live an active, fulfilling life after menopause. Remember, your bones are the foundation of your body – take care of them, and they will support you for years to come.

